
Dr. Kenneth Rosenthal
Dr. Jonathan C. O’Quinn
Dr. Michael J. Price

Dr. Kenneth Rosenthal
Dr. Jonathan C. O’Quinn
Dr. Michael J. Price


If your second toe seems to protrude a bit farther than your big toe, you might have what is commonly known as Morton’s toe. This condition may seem like a minor foot quirk, but it can lead to some uncomfortable problems. One of the primary issues associated with Morton’s toe is the increased likelihood of developing calluses on the sole of your foot and experiencing various types of foot pain. This happens because the longer second toe can alter how weight is distributed across your foot, putting extra pressure on certain areas. The condition is named after Dudley Joy Morton, who first described it in the 1930s, and is unrelated to Morton’s neuroma. In some cases, Morton’s toe can lead to more severe foot conditions, such as hammer toe or bunions, especially if your footwear does not accommodate your foot shape properly. If you are experiencing discomfort or noticing changes in your foot due to Morton’s toe, it is essential to seek help from a podiatrist who can offer various conservative treatments. These can include shoe modifications, custom orthotics, exercises, and medication, all of which can help to alleviate pain and prevent further complications. If you have Morton’s toe or are experiencing foot pain, it is suggested that you schedule an appointment with a podiatrist.
If you have any concerns about your feet, contact one of our podiatrists from Eastern Carolina Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Greenville, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics and its related study deal with the forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
Biomechanics and its related study deal with forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
The history of studying biomechanics dates back to ancient Egypt at around 3000 B.C., where evidence of professional foot care has been recorded. Throughout the centuries, advances in technology, science, and an understanding of the human body led to more accurate diagnosis of conditions such as corns for example. In 1974, biomechanics garnered a large audience when Merton Root founded Root Lab to make custom orthotics. He proposed that corrections of certain conditions could be implemented to gain strength and coordination in the area. Due to his research, we still use his basic principle of foot orthotics to this day.
As technology has improved, so have the therapeutic processes that allow us to correct deficiencies in our natural biomechanics. Computers can now provide accurate readings of the forces, movements, and patterns of the foot and lower leg. Critical treatment options can be provided to patients now who suffer from problems that cause their biomechanics to not function naturally. The best results are now possible thanks to 3D modeling and computing technologies that can take readings and also map out what treatment will do to the affected areas.
These advanced corrective methods were able to come to light thanks to an increase in both the technologies surrounding biomechanics and also the knowledge of how they work naturally. For example, shoe orthotics are able to treat walking inabilities by realigning the posture deviations in patients caused by hip or back problems. Understanding foot biomechanics can help improve movement and eliminate pain, stopping further stress to the foot. Speak with your podiatrist if you have any of these problems.

Diabetic foot infections are a significant concern for individuals with diabetes, often stemming from minor cuts or sores on the feet. These infections, which affect the soft tissue or bone below the ankle, can escalate rapidly and pose a risk of amputation if not managed promptly. They are typically caused by various bacteria, some of which are more challenging to treat. Approaches vary based on the severity of the diabetic foot infection and the patient's overall health. For more severe cases, hospitalization may be necessary, along with intravenous antibiotics. Assessing blood flow in the legs is imperative, particularly for those with circulation issues. Preventive measures play a vital role in reducing the risk of diabetic foot infections, including proper foot care, maintaining stable blood sugar levels, and avoiding smoking. Regular visits to a podiatrist for foot examinations are essential, and patients may benefit from wearing specialized footwear. To address concerns about diabetic foot infections, it is suggested that you include regular appointments with a podiatrist to assess your foot health.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Eastern Carolina Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Greenville, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.

Baseball players may experience various foot and ankle injuries, including contusions, fractures, heel spurs, and Achilles tendonitis. While these injuries can sideline even the most seasoned athletes, intervention from a podiatrist can make all the difference in swift recovery and long-term performance. Contusions are a common occurrence from ball contact or collisions among players. Sprains and fractures can occur during dynamic plays, such as sliding into a base, and require immediate medical attention. Catchers, who often bear the brunt of repetitive stress, can find relief from conditions such as plantar fasciitis and heel spur syndrome through custom orthotic devices and footwear recommendations provided by a podiatrist. By addressing issues like Achilles tendonitis with specialized care, including targeted stretching and strengthening programs, a podiatrist can help baseball players overcome injuries. If you incur a foot or ankle injury while playing baseball, it is suggested that you schedule an appointment with a podiatrist.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact one of our podiatrists of Eastern Carolina Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Greenville, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
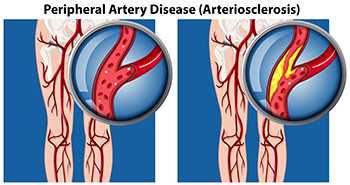
Peripheral artery disease, or PAD, is a common condition characterized by a buildup of fatty deposits in the arteries, resulting in restricted blood flow to the muscles in the lower legs and feet. A particular symptom of PAD is called intermittent claudication, which is a pain, cramp, or sense of fatigue in the leg muscles when you walk or exercise. Other symptoms are hair loss on the legs and feet, numbness or weakness, and slow-growing toenails. Leg ulcers, skin color changes, and shiny skin are other signs. PAD is primarily caused by atherosclerosis, where fatty deposits accumulate within arterial walls, narrowing the vessels. Contributing factors to peripheral artery disease include smoking, diabetes, high blood pressure, high cholesterol, and aging. Seeking help from a podiatrist is essential for an accurate diagnosis through physical examination and tests like the ankle brachial pressure index, or ABPI. Treatment involves lifestyle modifications, such as regular exercise, smoking cessation, and maintaining a healthy diet. In severe cases, surgical intervention may be needed to improve blood flow and alleviate symptoms. For help in determining whether you have peripheral artery disease that is affecting your foot health, it is suggested that you schedule an appointment with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Eastern Carolina Foot & Ankle Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Greenville, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
 Venous ulcers are open sores that often occur on lower legs and feet, due to poor blood circulation. Symptoms of venous ulcers include pain, swelling, and discolored or hardened skin around the ulcer. Podiatrists, or foot doctors, can help care for venous ulcers by offering treatments aimed at healing the wound, preventing infection, and improving circulation. This may involve cleaning and dressing the ulcer and prescribing compression therapy to reduce swelling and enhance blood flow. There may also be suggested lifestyle changes, such as regular exercise and elevating the legs to improve circulation. If you are struggling with wounds on the lower legs or feet it is suggested that you make an appointment with a podiatrist to get treatment and prevent future ulcers.
Venous ulcers are open sores that often occur on lower legs and feet, due to poor blood circulation. Symptoms of venous ulcers include pain, swelling, and discolored or hardened skin around the ulcer. Podiatrists, or foot doctors, can help care for venous ulcers by offering treatments aimed at healing the wound, preventing infection, and improving circulation. This may involve cleaning and dressing the ulcer and prescribing compression therapy to reduce swelling and enhance blood flow. There may also be suggested lifestyle changes, such as regular exercise and elevating the legs to improve circulation. If you are struggling with wounds on the lower legs or feet it is suggested that you make an appointment with a podiatrist to get treatment and prevent future ulcers.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Eastern Carolina Foot & Ankle Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Greenville, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.